Top 2024 Predictions for the Life Sciences, Pharmaceutical Industries
After the big changes in the life sciences and pharmaceutical industries in 2023, the new year promises continued challenges and more innovation.
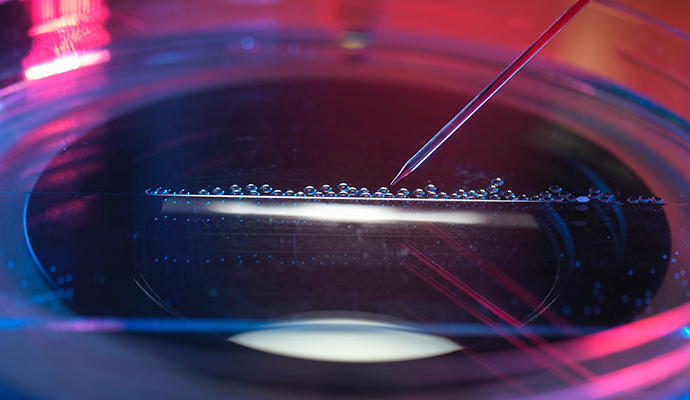
Source: Getty Images
- At the start of a new year, the life sciences and pharmaceutical industries face a roiling political climate, mental health crisis, and other challenges, but these industries are also riding a wave of innovation and technological advancements that could shift the tides.
The progress in cell and gene therapy is revolutionizing chronic disease care, especially for difficult fields like oncology. CRISPR has opened up new possibilities in sickle cell disease treatment and cell and gene therapy efforts have produced targeted cancer therapies. Additionally, male birth control is gaining ground, both in clinical trials and in popular opinion.
Partnerships will be key in 2024, particularly for overwhelmed pharmacies. And digital health will continue to evolve, particularly in the mental health space.
Alivia Kaylor: Hi, and welcome to another exciting episode of Healthcare Strategies. I'm Alivia Kaylor, senior editor of LifeScienceIntelligence and PharmaNewsIntelligence. Our brilliant associate editor, Veronica Salib, joins me today to discuss the current state of the life sciences and pharmaceutical industry in 2024. Veronica, thank you for joining me today. I'm so thrilled to be doing another well, the first episode with you.
Veronica Salib: Thanks. I'm really excited that we're doing one together too, especially considering how much time we spend talking about these things off-screen. And there's a lot of really exciting advancements that happened in the past year that are going to bleed into this coming year.
READ MORE: How Specialty Pharmacies Can Improve and Personalize Patient Care
Alivia Kaylor: For sure. Yeah, you're right. We spend so much time talking about this, just never on air, so I'm excited to dive into it.
Well, let's go ahead and start with a quick pulse check of the current state of the life sciences and pharmaceutical industry specifically. Veronica, what noteworthy advancements or breakthroughs have you observed through your reporting?
Veronica Salib: There's been a lot of really exciting advancements. We've reported on a lot of really exciting successes this year, and I think one of those areas where there's been a lot of success is in cell and gene therapy. As more and more treatments come to market as more research and funding is being allocated to these therapies, we're seeing more approvals.
Like this past year, Vertex and CRISPR collaborated on a gene therapy for sickle cell disease. It's a pretty groundbreaking medicine. It's the first one that we've ever seen that's been approved for gene therapy for sickle cell disease, which is going to make a really massive impact on the hundreds of thousands of Americans that are living with sickle cell disease.
Alivia Kaylor: I think it's personally exciting. I love CRISPR. I am so excited to see--I just actually wrote an article about CRISPR advancements that everyone should check out. Shameless plug here, sorry. But the CRISPR gene editing--I think it's so cool how it's being used to treat diseases. Definitely huge. It's come a long way from its first discovery in the late 1980s, so I'm sure that this breakthrough will profoundly impact patients' lives.
READ MORE: How Specialty Pharmacies Can Support Patients Managing Chronic Diseases
Veronica Salib: It's amazing how much we've been able to advance in the past year, not just in sickle cell disease, but even with applying cell and gene therapy in oncology. There have been a lot of really successful approvals in this past year and, beyond that, a lot of the people that I've spoken to recently who are experts in their field and who have really focused on cell and gene therapy are talking about how more and more researchers are looking for a way to manipulate the techniques that they've been able to successfully use in systemic cancers to attack solid tumors and to target the cancerous cells more specifically in those localized areas rather than throughout the whole body. And if we are to see that success, it'll be really exciting and it'll likely have [fewer] side effects because it's going to target that one area. And it might even be more successful than a lot of the chemotherapies that now just kind of function by erasing your entire immune system so that the body isn't attacking itself anymore, which is great that it helps cure the cancer, but at the same time, it causes so many side effects. It can cause hair loss, it can cause you to be more susceptible with infection. And right now with COVID and respiratory diseases on the rise, which we've talked about a lot, it really compromises that patient's ability to fight off these infections.
Alivia Kaylor: Well, this area is definitely promising. I'm excited to see more targeted therapies, more progress for solid tumors. It'll definitely change the oncology field, which will be inspiring to see. I know that so many have worked tirelessly to change this field, so I cannot wait to see what advancements come from 2024.
Veronica Salib: Absolutely.
Alivia Kaylor: And especially in cancer, because cancer treatments remain one of the biggest challenges in healthcare.
Veronica Salib: And I'm really excited to see how it specifically works for reproductive cancers and how it might be able to save some of the fertility that a lot of people lose when they're doing traditional chemotherapy or traditional treatments that they have to really plan ahead if they're planning on having their own biological children. And that can be very pricey, and it can be a very grueling experience. So if we can figure out a way to create more innovative treatments that help minimize those impacts, it'll be really exciting.
READ MORE: How Specialty Pharmacies Enhance Patient Outcomes with Digital Tools
Alivia Kaylor: Not only costly, but very costly for mental health, even, for those individuals. I can't imagine.
All right, well, let's move on to another area that I am personally excited about, which is male birth control. Given the reversal of Roe v Wade in 2022, I think there's been a renewed focus on contraceptive options for men. Veronica, you recently recorded a podcast on this topic, right? Can you share any updates with me?
Veronica Salib: Yeah, definitely. I think it's really important to preface that, right now, reproductive rights--reproductive healthcare, a woman's right to her own body and her decisions of what to do with it, whether or not they want to have a child--is so opaque, I think is the best way to say it, because turning it over to the states--every state has different laws. Every state has different jurisdictions. There have been recent court cases where people have been trying to get an abortion for safety reasons and have had to travel to a different state and have been denied that right by their state governments.
And so that has kind of caused people to look at the other side of the aisle, which is males and what their role is in pregnancy and bringing life to this world, and then preventing pregnancy. And I think you wrote an article a while back about shifting the burden of pregnancy prevention away from women and onto men a little bit because, up until this point, men have only had two birth control options, which [are] either a vasectomy or condoms. And condoms are effective and are helpful for preventing sexually transmitted infections and other things. And so they kind of belong in their own category, but they are not 100 percent effective.
And for women, it's often recommended to use two forms of birth control to kind of really minimize that risk of pregnancy. When women are taking on this role, they're carrying the mental load and then, on top of it, if [the birth control efforts] don't work and they do get pregnant, they're carrying the physical, the mental, the financial, all of these different loads. Those are really important things to bring into the conversation about male birth control.
I recently talked to Dr. Stephanie Page who's at the University of Washington, and she's working on multiple forms of male birth control--from hormonal forms, like a male birth control pill, to a gel that's called "NES/T gel," which uses testosterone and other chemicals to help prevent the body from producing sperm for certain periods of time.
She was really excited about those things, and that podcast will be coming out soon alongside an article. But she did mention that these gels are probably farther ahead on the pipeline than the male birth control pill. There's been a lot of kind of back and forth on the male birth control pill, and up until pretty recently, it's been kind of hard to find a ton of information on male birth control. There's been a lot more excitement now and focus towards it because men are realizing that they really have to play this big role, especially considering where we are in the political state of the world.
Alivia Kaylor: For sure. I hate to say it, but I think the reversal of Roe v. Wade kind of made some people rethink their family planning situation--or lack thereof, if you will. So I am personally excited to see these options.
I did an interview with the CEO of NEXT Life Sciences, and he is in charge of the Vasalgel, which is a hydrogel that's inserted or injected, if you will. And it's an alternative to a vasectomy because, I don't know if most people realize, but a vasectomy is not reversible always [or] a hundred percent effective. So it's providing a treatment for men and they don't have to worry. It's kind of like an IUD for women where it's in there, it's working, you can get it out when needed or when it expires--which I believe is 10 years for the Vasalgel--so, similar to Paraguard, the copper IUD. So it's cool that there's some equivalence for male and female birth control here. Do we know which method or do we want to predict which method will be the first to seek FDA approval?
Veronica Salib: So I think based on my discussions with Dr. Page, I really do think it's going to be the NES/T gel. Obviously, we don't know. They're still doing phase three clinical trials right now, but it's definitely a little bit farther ahead than some of the other ones. And then I think Vasalgel is definitely up there because they've been doing a lot of research with that as well. And that point you about vasectomy not being reversal is so important because right now the rhetoric on social media and other non-scientific sources is that "this is the catchall, this is the best option for men." And that's not necessarily true, especially for men who haven't thought about their family planning or that kind of aspect of their life yet.
Alivia Kaylor: For sure. And there [are] some physical side effects of vasectomy that maybe some people do not consider or even think of when undergoing this procedure. So I think that Vasalgel will provide a better alternative. I'd also like to talk about...you said the pill--I'm sorry, you said the pill was further along?
Veronica Salib: No, it's a little bit farther behind right
Alivia Kaylor: Now. Okay. That's right. That makes sense, because let's talk about taking a pill every day, right? It's hard enough for women to do, right? Do we think men want to take a pill every day?
Veronica Salib: It kind of just... That's a person-to-person thing. I know women who are very strategic about "I take my pill at the same time every single day," and then I know women who are just like, "yeah, sometimes I remember to do it, sometimes I don't" and it's kind of a hit or miss--which don't do that. If anyone's listening and they do that, please stop doing that.
But I do think that the benefit of having something like Vasalgel, which lasts 10 years, is that they don't have to think about it. They don't have to worry about, "am I taking it effectively? Am I doing it correctly? Did I miss it? Did I bring it with me?" Also for talking about costs--an upfront cost of a procedure like that versus paying for 10 years worth of birth control pills...I don't know the exact math, but I can imagine that there might be a benefit to doing it once and then having it for 10 years and then reversing it. Obviously, we don't know what that's going to cost right now, but I do think that's a conversation worth having.
And then there's the access issue. A lot of women have trouble accessing oral birth control pills because either they don't have insurance coverage, they can't find the right one for them because there are so many different kinds of female birth control. Having a procedure that's just kind of one and done, kind of like the way the IUD offers it for women, you can have it for so long and you don't have to worry about finding another physician or getting the prescriptions or paying for the prescriptions, or, if you switch your insurance, "will the insurance cover this prescription?" And there's just a lot of other factors that you have to consider when taking a pill versus "one and then I'll have it for a while and when I'm ready to talk about having kids or if it expires, I can just go back to another physician," which is kind of ideal in that scenario.
Alivia Kaylor: Yeah, for sure. Okay. Well, we should move on. I could talk about this all day, but let's talk about the regulatory landscape. We all know that the regulatory environment is always a hot topic. Have there been any recent changes or updates that our audiences should be aware of?
Veronica Salib: Yeah, so this past year has been a little bit of a feat for the FDA and the regulatory environment. There have been a lot of successes. We've seen a lot of the cell and gene therapy approvals. Those things are very exciting.
But we've also seen a lot of recalls. On PharmaNewsIntelligence, we did a whole article about the eyedrop recalls, and that was kind of jarring to see how many--I think it was, at the time of writing that story, it was like 26 different eyedrops have been recalled over the counter. There was one prescription, I believe. But these are from brands that are widely known. It's not some sort of off-brand eyedrop that you're like, maybe you shouldn't have been putting that in the first place. But places like CVS, like Walmart, these big retailers were selling these eyedrops that were contaminated.
And the question is, how did they even get to the market? Is the FDA regulating it well enough? Is there a problem with imports, because a lot of these were manufactured overseas? There's a lot of big question marks right now. And are these companies following current good manufacturing processes? And spoiler alert, they're not. A lot of the FDA investigations have shown that there have been really kind of scary violations in these manufacturing facilities, things that are not sterile, that should be. And with eyedrops, there is the kind of risk of touching your eye and contaminating the drops that way. But--from the research that I've seen and from the reporting that I've seen from other sources and the reporting that we've done--that has not counted for a lot of these infections that people are experiencing.
And then anyone who's arguing that this is unique to eyedrops has to look at kind of the broader scope of things. We've had a lot of infant formulary recalls, which, again, very scary because this is a very fragile population that uses this stuff. And especially with recently, I can't remember the exact name, but they recalled an infant formula that was used for a lot of infants with dairy allergies. And we don't know exactly what other exposures could be dangerous to this particular group of babies and patients. So that's a concern.
And then in the medical device space, there's also been quite a few recalls of BiPAP and CPAP machine masks with certain metals that can interfere with pacemakers, certain metals that can interfere with the way the actual machine is functioning.
All these things require their own episode where you can sit down, pick it apart, and see where exactly everything went wrong. But I think it points to a bigger issue of how we're regulating these things and why we're not catching them earlier on, and there needs to be a little bit more attention on it. And we need to figure out a way to test these things early on, make sure that we're not recalling hundreds of batches of these products because not everyone's getting that information. Unfortunately, you and I--we do a lot of reading in this industry [and] a lot of the providers we talk to, they're staying up to date because it's their industry, but the average consumer, unless it appears in some sort of mainstream media that they read or see, they're not going to know about these recalls until something happens.
Alivia Kaylor: It's really unfortunate, and I feel like the answer is more quality control here.
As you know, I was previously employed by a pharmaceutical company that specialized in sterile injectables, and I worked as a microbiologist and an environmental monitor. My job--it was making sure [of] sterility, number one, right? We're filling injectable drugs and they have to be sterile. There can be no contaminants in these at all. And there's a lot of protocols, a lot of good manufacturing practices that need to be followed. And if those are not followed, they lead to deviations. You don't want deviations. And then lead to investigations. And that's where I think the root of this is. I don't know if it's maybe the people who work in these pharmaceutical industries aren't getting enough breaks. They aren't getting enough time to do what they need to, so they're rushing through skipping steps. That will always lead to problems.
Another thing though is I think that these need to be caught more by the FDA. I was part of several FDA checks at the pharmaceutical manufacturing plant that I worked at, and I personally felt like they weren't thorough enough. I'm interested to see how the FDA changes, maybe, their investigative tactics or how they have decided to explore these facilities.
I just think that something needs to be done here because these recalls, they're alarming. And as you said, some of them are very vulnerable populations.
Veronica Salib: Yeah, and then another thing I forgot to mention, especially with the ophthalmic drugs, it's kind of already surpassing your body's natural fail-safe. It's going directly into your eyes. So that's another big concern.
But like you said, there needs to be a way for these inspections--or these audits or whatever it may be--to provide a better picture of what is happening year-round. A company can't be doing pristine and stellar for their audit, and then a couple of months later have a bunch of recalls. Obviously, there's something that's not adding up there, for lack of a better term. How are we making sure that they're following these processes year-round constantly? Are we doing more regular checks? Is there an FDA person that is on staff for a certain area of the world and they go regularly check these facilities? Is there certain reporting that they have to do? How are we making sure that the reporting is accurate?
Unfortunately, a lot of these companies are a business, so their primary goal, their bottom line is to make certain funds. And while they do have other goals and they do great things for the healthcare industry, we need to figure out how they weigh the benefits and the costs because that'll make a really big difference in how we monitor and regulate them.
Alivia Kaylor: Sacrificing cost savings and risking patients' lives just ain't it.
Alright. Well, let's move on to collaboration and partnerships, something that we're seeing kind of play out in real-time here. Veronica, if you want to elaborate on this....
Veronica Salib: Collaborations and partnerships between different companies, between institutions, between nonprofits, between healthcare facilities [are] so important for advancing healthcare. No company's going to have all the resources to do everything that they want to do, and that kind of happens the same with other issues.
Right now we're experiencing a blood shortage, a major blood shortage. We don't have enough donors. And with COVID and all the different things that COVID caused, a lot of people who normally would donate aren't donating as much. And right now, the American Red Cross and other blood collection organizations are working together to kind of figure out how they can leverage new technologies, remote discussions about how they can improve the blood donation process, make it easier for donors, and maybe get more donors out there. Because unfortunately, if you can't get people to go to the donation center or if you can't bring the donation center to the people who are donating, we are going to continue to be at a loss. And that is going to cause a lot of problems for surgeries, both elective and necessary surgeries. It's going to cause a lot of problems for people who have chronic diseases and chronic conditions that may require regular transfusions. So right now, I believe you published an article recently about how the American Red Cross is leveraging social media and personalized communication and engagement strategies to bring in donors and kind of maintain that adequate blood supply, which we unfortunately don't have right now.
Alivia Kaylor: Yeah, and that's such a good point. I work remotely now, but my previous job, I worked in an office and I donated regularly. And my last New Year's resolution was to donate more and I only ended up donating three times, and that's less than I usually donate, which is horrible. I am even struggling now because I have to actively make appointments. That being said, I'm donating tonight with my neighbor.
So everyone listening, if you can, if you're eligible, please donate. Please, please. It is such an urgent need and it is so needed and appreciated. And if you have the American Red Cross app, they will actually give you in real-time where your donation is, and then when it lands to a patient, it tells you what location your blood was sent to, and you can save up to three lives with just a pint blood, one donation. Platelets are also needed. It's really cool to see what American Red Cross is doing with the outreach and the digital platforms. It seems like they're really getting, if you will, getting hip with it and hopefully it works out.
Veronica Salib: And definitely speaking to eligibility, we've recently expanded some eligibility. People who have different sexual orientations who previously weren't allowed to donate, the restrictions have changed a little bit for that. So I think it's important, even if you weren't eligible before, to reevaluate and see if maybe you're eligible now. Because I think a lot of people, if they go once and they're not eligible, they're like, "well, I can't do it again." But guidelines are changing, your body is changing, so you may be able to this time around. It doesn't ever hurt to go in and get tested and see if you are eligible.
Alivia Kaylor: Yeah, for sure. And I will say through the emails and outreach that I've been receiving from the American Red Cross, it seems like some of the rewards for donating have been pretty hefty.
Alright, well, let's move on to provider burnout and mental health, which is huge. Have there been any developments or initiatives to address these challenges that you've been seeing through reporting?
Veronica Salib: There have been some things. Mental health and burnout is kind of my wheelhouse, is where I am very interested in seeing what advancements have been made. And with the COVID pandemic, despite the national emergency ending, hospitals are still inundated with the amount of covid patients. Respiratory disease patients and providers are unfortunately bearing a lot of the brunt of that. They are having to work more hours. They are--pharmacies, especially, pharmacists are so important in this discussion about burnout because so often they're left out, but pharmacies are so short-staffed. They can't really find enough people to keep up with the demand of drugs that we need, the demand of filling and stuff like that.
I recently had an experience at a pharmacy where I went in and--it was an interesting experience all around, but one of the things that I noticed was that they only had two techs working. And when I spoke to the tech, they were like, "yeah, we're supposed to technically have six on staff," but the holiday season with the fact that they're short-staffed, they're just running at a slower pace. And so it was taking them a lot longer to fill the prescriptions that they needed.
But there have been initiatives that have been working towards improving this. One of the things that I think is really important is automating what can be automated. So certain things, especially in the pharmacy, can be automated. There are administrative tasks that can be streamlined a little bit better. And so that way the provider isn't feeling like they are spending 90 percent of their day clicking check boxes or assigning papers or things like that.
Obviously, there always needs to be a human in the loop and there needs to be some oversight to make sure that there aren't any errors and there's a reason that we have those systems in place and why it is so taxing because we want to make sure we're keeping patients safe. But there's a way to manipulate that a little bit and make it a little bit easier, maybe do additional trainings for pharmacy techs, allow them to take over some of the administrative roles so that the pharmacist can focus more on their more clinical tasks, whatever that may be.
And again, pharmacists play such a crucial role. They administer a lot of vaccines, which has been so important in the past couple of years. It's important all the time, but especially in the past couple of years. So there's been that, and there's also been some discussions about flexible scheduling, allowing providers with a little bit more time when it comes to scheduling, allowing them to counsel patients and to be able to bill that.
And I think there's a whole other discussion that can come with insurance and what providers can and cannot bill for and what they aren't aren't being reimbursed for, which is again, a whole other conversation that I will not dive into right now. But I think that those are discussions that are important to have in the longterm and important so that the provider feels that they're fulfilled.
I recently spoke to a healthcare provider who talked to me about physician burnout, and she mentioned that the feeling of burnout comes when you're no longer fulfilled with the position that you are doing. There are a lot of different angles you can come at provider burnout from, but definitely it's been nice to see that more health systems have been talking about burnout and mental health for physicians and for attendings and residents especially. Residency is so taxing from what I've seen, what I've read, what I've heard. And so it's important that they have these resources and can access them without fear of retribution. And how each health system deploys that is dependent on how they function, and it's dependent on what their individual staff needs. Because in rural communities where staff might need to reach patients that are living very far and broad from each other, it may be different than in a more urban hospital setting where the patients are readily coming to them, but they don't maybe have enough time to see as many patients as they have in their ER or in their waiting room. So yeah, a lot of different angles on that one.
Alivia Kaylor: Yeah. Well, thanks for sharing that. Before we wrap up, let's go ahead and talk about sustainability and social responsibility. Currently, as it stands, the healthcare industry accounts for about 8.5 percent of all greenhouse gas emissions in the US and about 4.5 percent of worldwide emissions. I know that doesn't seem like a lot, but that is still a higher number than we would like. So I would love to know about what these organizations are doing to combat this number and what they're doing to decrease their emissions.
Veronica Salib: Yeah, so definitely I think sustainability is becoming increasingly important to these companies, and a lot of them are touting how they are recognizing their social responsibility, the impact they're making on the environment, how they might be adopting environmentally friendly policies. So some of them may be looking at more sustainable packaging, energy optimization with how the facilities function or more environmentally friendly manufacturing practices.
But I do think right now there isn't enough information from these companies on what exactly they're doing. We want to see the details, we want to see the numbers, we want to see the stats. And I know you've had a little bit of trouble finding people who are willing to talk about sustainability, especially in the pharmaceutical industry.
Alivia Kaylor: Yeah, absolutely. It's been a bit of a pulling teeth adventure, trying to find someone to speak about this. And I'm not sure if that is, maybe it's a newer field, chief sustainability officers. I don't know if that's maybe too new of a position or if...I don't know. I don't know what's going on here.
But this is a call to action for my audience. If anybody is a sustainability expert in the healthcare industry and you want to speak to me, I definitely want to speak to you. So reach out. I'll give you email information at the end of this episode and hopefully I hear from you.
But yeah, I would just love to see more sustainable initiatives roll out, especially with how much plastics being used, logistics, reducing waste. I know some medical devices have been curated to reduce waste, mainly making it able to be sterilized and reused or things like that, which are great to see. So I hope more organizations rely on sustainability and keep that in mind as they continue to make treatments and devices.
Veronica Salib: And I think it's important to point out that when we talk about sustainability, we're not saying everything should be reusable because some things need to--the only way that they can be sterile is for it to be single use. And I think that's such a common misconception when discussing sustainability in healthcare. That's not what anybody's saying, but it's how can we get as little as possible of waste or as little as possible of greenhouse gas emissions or getting it as low as we can possibly get it.
Alivia Kaylor: That's a good point. And this is my wheelhouse, especially [with an] undergraduate in microbiology, master's degree in sustainability. I understand sterility, and I also understand that we need to reduce emissions. And that's a good point. For example, in a cafeteria of a hospital, single use plastics do not need to be used. You can have compostable forks. Should we have compostable forceps in the operating room? I don't think so, but you know what I mean, choose your battles here. There's logistical ways of doing this, and I'm excited to see what type of innovative tactics come from this.
Veronica Salib: Me too.
Alivia Kaylor: Alright, well, we have to wrap up our episode. So thank you so much for joining me today, and thank you for sharing all of your insights, Veronica.
Veronica Salib: Thank you. This is fun. Just like our normal chats.
Alivia Kaylor: I know it was fun, although this is very PG. I like it.
As for our listeners, we'd love to hear from you. Feel free to contact me with any healthcare-related questions or subjects you think we should cover by emailing me at a-k-a-y-l-o-r@techtarget.com. And if you like this episode, please consider reading or reviewing us on Spotify, Apple Podcasts, or wherever you're listening. Thanks for tuning in. We'll be back soon.
