How the Delta Variant Exacerbates Healthcare Disparities
Disparities between rural and urban healthcare predict the worst outcomes of COVID-19’s Delta variant, found a recent Data Insight from Xtelligent Healthcare Media.
Source: Source: Getty Images
- The fast-spreading Delta variant is the dominant strain of a virus many had hoped would be eradicated by now. COVID-19’s Delta variant was first identified in India in December of 2020. Now Delta accounts for 97 percent of new infections in the United States, according to data from the Centers for Disease Control (CDC).
The growing impact of Delta on the US is reminiscent of March 2020 when hospitals were overwhelmed with patients and many businesses closed their doors. Moreover, Delta is twice as contagious as past variants making it the fastest and fittest variant to date according to the CDC.
Mutations to the SARS-CoV-2 genome have increased Delta’s transmissibility and quickened the pace of its replication in the body. Studies show that Delta tends to result in more severe outcomes for those who are unvaccinated, while hospitalizations remain low for fully vaccinated individuals.
Initial understandings of vaccine efficacy suggest that one dose of either the Moderna or Pfizer vaccines are 18 percent less effective against Delta (30.7%) than they are against the Alpha variant (48.7%). Still, two doses of these vaccines are only slightly less effective against the Delta variant (88%) compared to the Alpha variants (93.7%).
Some nations are now administering booster shots and increasing mask mandates to manage changes in vaccine effectiveness, yet the US remains slow to offer boosters or change COVID-19 guidance.
The culmination of new data prompted CDC director Rochelle Walensky MD to comment that “this is becoming a pandemic of the unvaccinated.”
Delta’s contagiousness makes it responsible for many of the breakthrough cases that have begun to crop up among vaccinated populations. The variant’s high viral load can cause symptoms in vaccinated individuals, making them contagious to other vaccinated or unvaccinated people.
Compared to less developed countries with lower vaccination rates, most of the US has little to worry about when it comes to a possible overwhelming virus surge. The United States has fully vaccinated 50 percent of its population with another 9 percent receiving at least one dose as of August 2021.
However, when compared to peer countries, the US still lags in vaccine administration. This discrepancy can be explained in part by the disparities between vaccination rates in different parts of the country.
The risk of severe outbreaks is compounded in communities with low vaccination rates because of existing disparities in hospital capacity. Decreased regulation and large gatherings bring more highly vaccinated communities into contact with unvaccinated groups. Vaccinated individuals are at an increased likelihood of becoming infected with the Delta variant and unvaccinated individuals are now more likely to spread the virus exponentially in their own communities.
This type of community outbreak is known as “hyperlocal,” according to a recent article from Yale Medicine. In these situations, the virus skips from one poorly vaccinated area to the next. Consequently, healthcare systems in these areas may quickly become overrun by the influx of Delta variant cases if they lack proper resources.
Rural areas make up the bulk of communities with low vaccination rates and existing healthcare disparities. Vaccination data from the CDC found that adult COVID-19 vaccination coverage was lower in rural areas (38.9%) than in urban areas (45.7%) as of April 10, 2021. And vaccine hesitancy is higher in rural counties showing that rural residents are more reluctant to be vaccinated than urbanites.
Persistent vaccine hesitancy and comparatively lower hospital capacity put rural areas at a high risk of hyperlocal outbreaks.
Rural care settings have only 1.7 ICU beds per 10,000 people, whereas urban settings have 2.8 ICU beds per 10,000 people. Disproportionate accessibility to care is representative of urban counties’ superior ability to react to outbreaks in their jurisdiction when compared to rural counties.
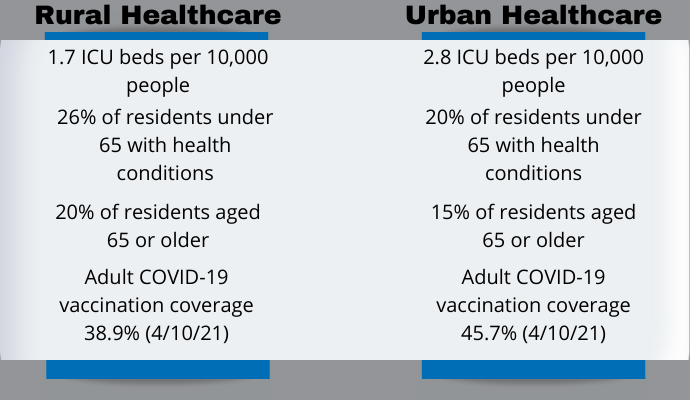
Source: Xtelligent Healthcare Media
Rural counties are also older, with 20 percent of the population aged 65 and up, compared to urban areas at 15 percent. Rural areas tend to be sicker as well, with 25 percent of individuals younger than 65 having some underlying medical condition, versus 20 percent for urban citizens under 65. Both demographics increase the risk of a rural populous being more adversely affected by a Delta variant outbreak than an urban one.
To assess the threat of hyperlocal outbreaks to rural areas, Insights by Xtelligent Healthcare Media analyzed healthcare system disparities. Data from “covidcaremap” was combined with local-level CDC data to identify 350 US counties that are most at-risk for severe Delta outbreaks if vaccination rates do not improve.
Analysis revealed that 21 percent of 1,560 rural counties are at very high concern for COVID-19 outbreaks. Meanwhile, only 14 percent of 960 urban counties were categorized as also being very high concern. In a statistical analysis, these results were significant. If a hyperlocal event were to occur, these rural counties are not likely to be able to deal with the fallout.
The 350 rural counties Insights found to be at risk have less than 1.7 ICU beds per 10,000 individuals and their county-level CDC vaccination rate is below 30 percent. A few areas including Texas, Hawaii, and disparate counties were not reported in the data.
In the case of another COVID-19 wave, these rural counties may be on the front line unless vaccines can be administered effectively.
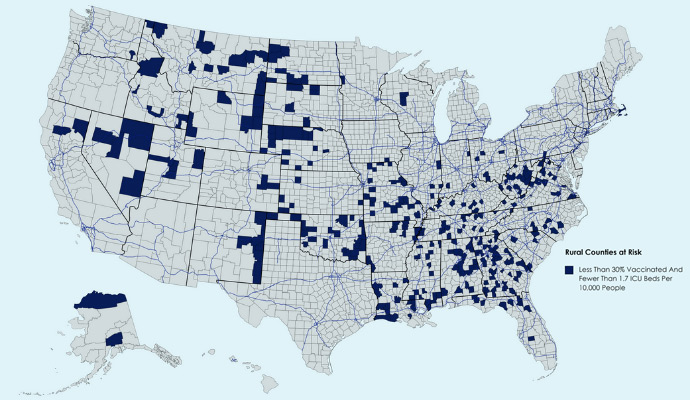
Source: Xtelligent Healthcare Media created with mapchart.net
As variants of the coronavirus spread simultaneously with reduced COVID-19 restrictions, the most vulnerable areas should be supported with the best medical resources available. Rural counties are now the most susceptible to Delta variant outbreaks because of low vaccination rates and healthcare shortfalls.
To avoid hyperlocal events, vaccine efforts must be increased where access is limited. Resources should also be redirected to account for overwhelmed rural healthcare systems. Without bolstering community vaccination efforts, frontline workers are at risk for burnout as the disease spreads unabated. By using county-specific data, professionals can prepare their healthcare systems for hyperlocal events, and educate their communities about the risks at hand.
