Skilled Nursing Facilities Are Facing a Staffing Crisis
Skilled nursing facilities are facing a rising staffing shortage on every front and a new CMS mandate stands to exacerbate the problem.

Source: Getty Images
- Staffing issues at skilled nursing facilities are threatening patient health and the industry’s future. Hundreds of thousands of employees have left jobs in nursing homes, and shortages may be intensified by a Centers for Medicare and Medicaid Services (CMS) vaccine mandate. Skilled nursing facilities and their patients are in jeopardy if this mandate leads to more nurses, aides, and other staff leaving the industry.
A Staffing Problem
The coronavirus pandemic has exacted a burden on healthcare workers for nearly two years, and those working in skilled nursing facilities have faced extreme hardship because of the vulnerabilities of their patient population. Overburdened and often underpaid, many thousands of skilled nursing facility employees have elected to leave their jobs and seek work elsewhere. Labor statistics from the St. Louis Fed find that 400,000 people have left jobs in the nursing and residential care facility sector since the pandemic’s start, bringing the total number of employees down to levels not seen since July 2007.
To understand the extent of the nursing home staffing crisis, Insights by Xtelligent Media used comprehensive CMS nursing home data from approximately 15,000 skilled nursing facilities. The self-reported data collected over the past two years shows that these facilities are not recovering staff lost during the pandemic. Moreover, data also reveals that facility employees remain unvaccinated at high rates, which is especially troublesome considering the recently approved CMS vaccine mandate that now threatens to compound skilled nursing facility staffing shortages and result in a crisis for patients.
Source: Xtelligent Healthcare Media
By the Numbers
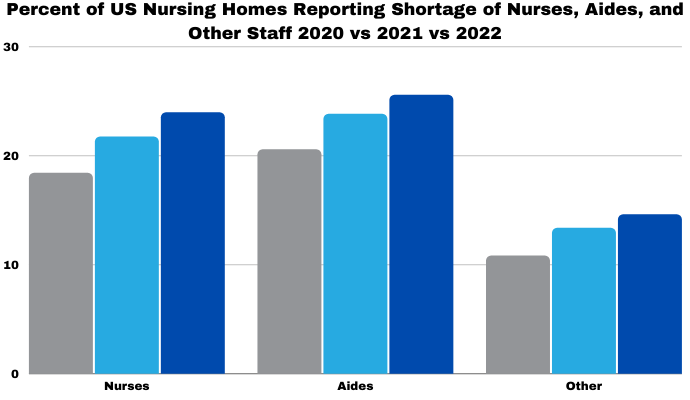
Skilled nursing facility data from November of 2020, November of 2021, and the first month of 2022 all indicate that the pandemic staffing crisis is not halting. The first collection of data from 2020 shows that 18 percent of US facilities were suffering from a shortage of nurses. During the same month of the following year, 22 percent of facilities were experiencing shortages and nearly one-quarter of all facilities claimed a nurse shortage in the first month of 2022. This amount of insecurity is a danger to patient health, but some areas of the country are suffering even worse rates of shortage.
Staffing shortages lead to worse patient-provider ratios. Higher rates of medical error, provider burnout, and morbidity result when these patient-provider ratios fall below optimal proportions. An increase in turnover of the profession is also difficult to manage for administrators and can create dysfunctional care settings.
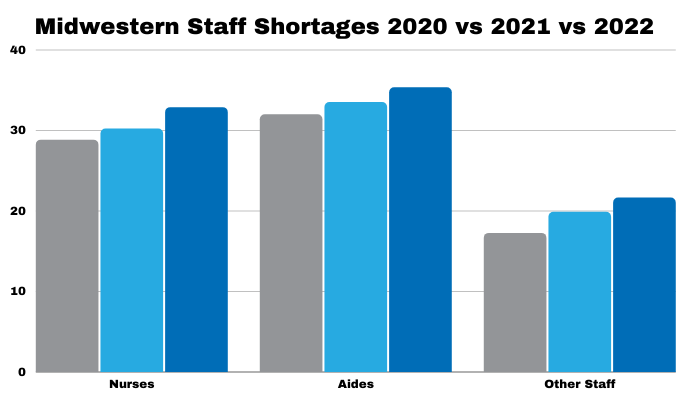
Midwestern states—as designated by the US Census Bureau—are significantly understaffed. A third of Midwest facilities have reported a shortage of nurses as of January 2022. The same facilities are reporting a 35-percent aide shortage and 22-percent shortage of other staff. These numbers represent a 4-percent increase in reported nurse shortages, a 3-percent increase for aides, and a 4-percent increase in other staff between now and November 2020. These high rates of staffing shortage for nurses and supporting positions like aides, medication technicians, and custodial employees can contribute to increased mortality rates in nursing homes.
Source: Xtelligent Healthcare Media
Other staff—like custodians or administrators—and aides are experiencing a nationwide surge of shortages. Facilities are reporting a 5-percent increase in the rate of aide shortages since November of 2020, with one-quarter of nursing homes now claiming a shortage. Nursing homes have experienced similar shortages with other employees, where 15 percent claimed a shortage in 2022 compared to 11 percent in November 2020. Accordingly, skilled nursing facilities must maintain the remainder of their workforce.
Nursing homes are encouraging vaccinations and providing testing for all people in their facilities to avoid the coronavirus infections that could worsen an already severe staffing shortage. Analysis of CMS data shows that 98 percent of all facilities can test their staff. The Northeast census region has the lowest average ability to test at 97.5 percent.
However, vaccinations are not as common as tests in skilled nursing facilities. Staff is vaccinated at an average rate of 80 percent across the nation, but in Midwestern and Southern nursing facilities, staff were vaccinated at 73 percent and 77 percent, respectively.
The CMS mandate recently upheld by the US Supreme Court threatens to cut the staff in some of these skilled nursing facilities and extend the already dangerous shortage. Updated guidance from CMS would monetarily penalize nursing homes if their staff remains unvaccinated. Facilities that do not have vaccinations by February 25 may even lose their Medicare and Medicaid contracts.
A successful mandate rollout could increase strain on skilled nursing facilities. For example, New York’s vaccine mandate grew the percentage of vaccinated staff by roughly ten percent and other mandates have increased the total percentage of vaccinated staff to around 90 percent. While this is beneficial, nursing homes can’t stand to lose 10 percent of their nurses, aides, or other staff because of their vaccination status.
Breaking the Pattern
Skilled nursing facilities throughout the US are struggling to maintain their essential staff. These shortages are harmful to patients’ health and may increase mortality rates. If the CMS vaccine mandate compounds this staffing problem, the situation for patients in some regions may become worse.
While most nursing facilities have high availability of tests for residents and personnel, they don’t have high vaccination rates. Thus, CMS should be cognizant of the unintended consequences of their mandate and offer an alternative testing program that does not enforce penalties for nonvaccinated employment. A dire situation may be made worse for patients if they do not consider these types of alternatives.
